Microbiology Lesson – 10: Antibiotic Sensitivity Test Protocol
Welcome to the tenth lesson in our microbiology series! In this lesson, we will be discussing the protocol for conducting an antibiotic sensitivity test. This test is crucial in determining the effectiveness of different antibiotics against specific bacteria.
1. OBJECTIVES
• To utilize specific monitoring techniques to evaluate the susceptibility of a microbe to different antibiotics.
• To distinguish the range of activity of an antibiotic
• To determine which antibiotics or antimicrobial drugs are effective in treating an infection caused by a specific strain of bacteria, fungi, or other microorganisms.
2. INTRODUCTION
There is a large number of antimicrobial agents available for treating diseases caused by microorganisms. Such drugs are now an essential part of modern medical practice. The antimicrobial agents used in medical practice are aimed at eliminating the infecting microorganisms or at preventing the establishment of an infection. As a rule, antimicrobial agents are of most use in medicine when the mode of action of the antimicrobial chemicals involves biochemical features of the invading pathogens not possessed by normal host cells.
3. PURPOSE
Identify Effective Treatment: Determine which antimicrobial agents are most likely to effectively treat an infection caused by a specific microorganism.
Guide Antibiotic Selection: Assist healthcare providers in selecting the most appropriate antibiotics or antifungal to target the infection, thereby minimizing the risk of antibiotic resistance.
Monitor Resistance Patterns: Track and monitor patterns of antimicrobial resistance among microorganisms, aiding in public health efforts to combat resistant strains.
1. Sample Collection:
Collecting a urine sample for isolation and identify bacterial infections in the urinary tract. Here’s a step-by-step guide on how to collect a urine sample for culture:
a) Materials Needed: A clean, sterile urine specimen container, Disposable gloves, Soap and water
b) Procedure: Begin to urinate into the toilet or a clean container. About halfway through the urination process, stop for a moment. Position the sterile urine specimen container under the stream of urine to collect the midstream sample. Continue urinating into the container until it is about half full (usually 30-60 ml). Cap and Label the Container: Close the lid of the urine specimen container securely to prevent leakage. Label the container with the patient’s name, date, and any other relevant information requested by the healthcare provider.
Isolation of Bacteria from Urine Sample
Bacteria isolation refers to the process of obtaining and growing a pure culture of a specific bacterium or group of bacteria from a mixed population. This is done to study, identify, and characterize the particular bacterium of interest. Isolating bacteria involves separating them from other microorganisms or contaminants, allowing researchers or microbiologists to analyze their characteristics, behaviors, and properties more accurately.
The isolation of bacteria typically involves several steps:
Inoculation
Incubation
Colony Formation
Selection
Inoculation : The collected sample is streaked onto a culture medium MacConkey Agar plate that provides the necessary nutrients for bacterial growth
Incubation: The culture medium with the sample is placed in a controlled environment, usually at a 35-37 C temperature and humidity, to encourage bacterial growth.
Colony Formation: Bacteria in the sample will multiply and form colonies on the culture medium. Each colony represents a single type of bacterium.
Selection: A single colony is selected and transferred to a new culture medium to ensure a pure culture. This process repeated four times to achieve a high level of purity.
: Identification of Micro-organism of isolated colony :-
Generally, they involve a combination of Gram staining, culture
colony morphology, and biochemical tests. As the different tests are
carried out, the results obtained narrow the possible options until
identification is obtained.
Study of Colony Morphology
Study of Bacteria morphology via Gram staining
Biochemical Identification of micro organism
-: Identification of Micro-organism of isolated colony :-
“Colony Morphology”
The isolated colony morphology of bacteria on MacConkey agar is
pink to dark pink, dry, and donut or circular-shaped, with 2–3 mm
Size and structure is Opaque. The colonies are surrounded by a dark
pink area of precipitated bile salts. They appear flat and have a
smooth, entire margin. The colonies are lactose fermenting.
According to colony morphology E. Coli bacterial may be formed
this colony.
The colonial characteristics described only give a presumptive
identification of the isolated organisms.
-: Identification of Micro-organism of isolated colony :-
“Gram Staining”
Cells are typically rod-shaped, gram-negative, straight, rod-shaped,
non-acid fast, and bacilli that exist in single and pairs. The
morphology of bacteria exactly matched with E. Coli Bacteria
Morphology.
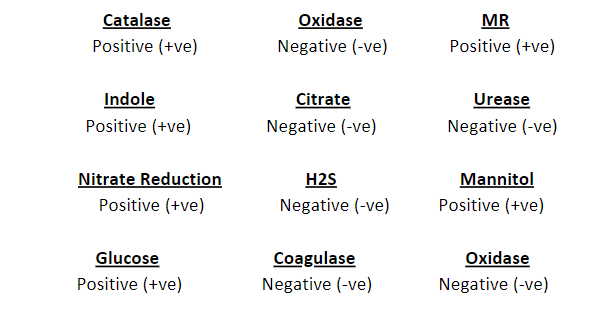
-: Identification of Micro-organism of isolated colony :-
“Biochemical Identification of Microorganism”
Biochemical tests identify bacteria by observing the enzymes they
produce. Bacteria produce large amounts of enzymes, and the type
of enzymes they produce can be used to classify their species.
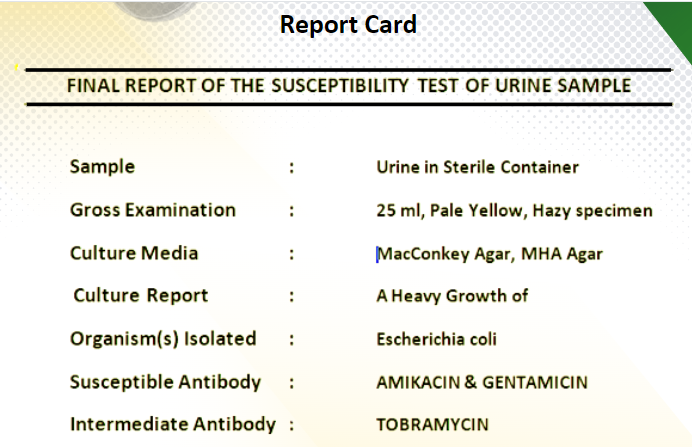
After colony morphology study, gram staining and biochemical identification of the isolated colony is E Coli bacteria.
-: Antibiotic Susceptibility Testing Procedure :-
Antibiotic susceptibility tests identify the pathogen and the
antibiotics that are likely to inhibit its growth. The most common
methods for in-vitro antimicrobial susceptibility testing are: Disk
diffusion, Agar dilution, Broth macro dilution, Broth micro dilution,
Concentration gradient test.
In this project we are follow Disk Diffusion method also known as
the agar diffusion test, Kirby–Bauer test, disc-diffusion antibiotic
susceptibility test, disc-diffusion antibiotic sensitivity test and KB
test
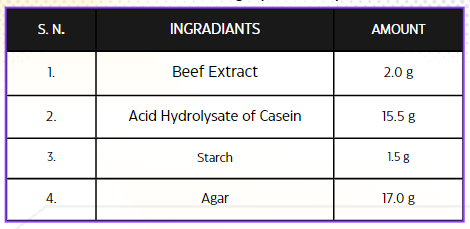
-: Antibiotic Susceptibility Testing Procedure :-
“Preparation of Mueller-Hinton Agar Plate”
Formula for Mueller-Hinton agar per liter of purified water
Antibiotic susceptibility tests identify the pathogen and the antibiotics that
are likely to inhibit its growth. The most common methods for in-vitro
antimicrobial susceptibility testing are: Disk diffusion, Agar dilution, Broth
macro dilution, Broth micro dilution, Concentration gradient test.
In this project we are follow Disk Diffusion method also known as the
agar diffusion test, Kirby–Bauer test, disc-diffusion antibiotic
susceptibility test, disc-diffusion antibiotic sensitivity test and KB test
-: Antibiotic Susceptibility Testing Procedure :-
“Inoculation of the MH plate”
1. Dip a sterile swab into the inoculums tube.
2. Rotate the swab against the side of the tube (above the fluid level) Using firm
pressure, to remove excess fluid. The swab should not be dripping wet.
3. Inoculate the dried surface of a MH agar plate by streaking the swab three
times over the entire agar surface; rotate the plate approximately 60 degreeseach time to ensure an even distribution of the inoculums.
4. Rim the plate with the swab to pick up any excess liquid.
5. Discard the swab into an appropriate container.
6. leaving the lid slightly ajar, allow the plate to sit at room temperature at least
3 to 5 minutes, but no more than 15 minutes, for the surface of the agar plate to
dry before proceeding to the next step.
-: Antibiotic Susceptibility Testing Procedure :-
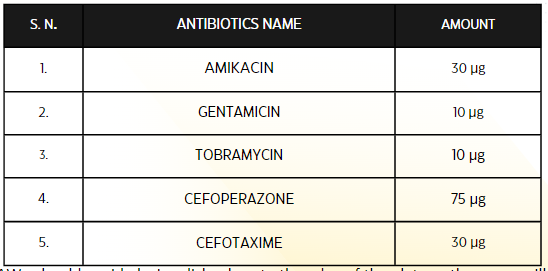
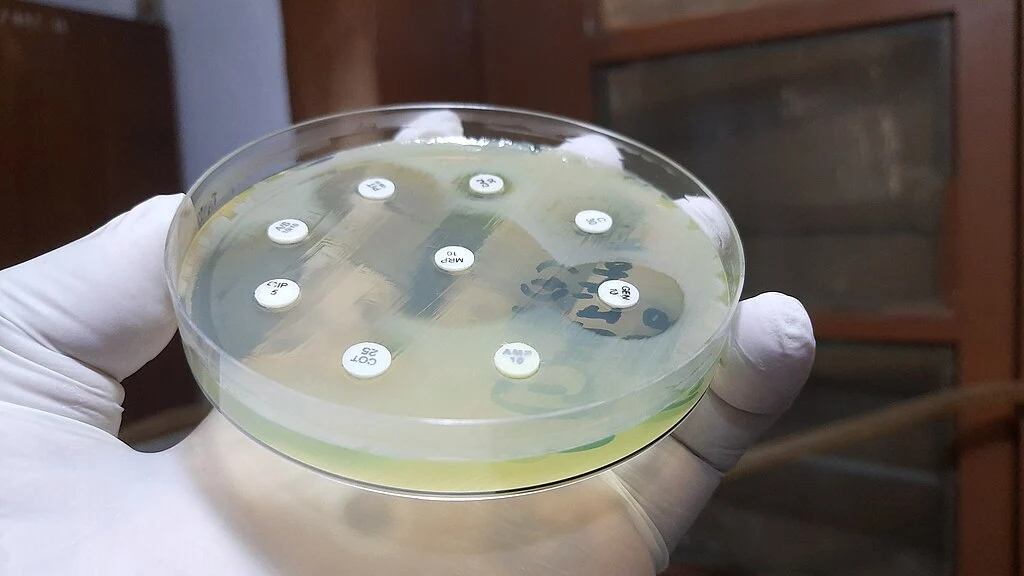
“Disk placement”
Manual disk placement for eight disks on a 100-mm plate. Using sterile forceps
carefully place the selected antibiotic disks on the surface of the agar plate. Gently
press down on each disk to ensure contact with the agar surface, but do not push it
too far into the agar.
List of Antibiotic Disc used on the MHA Plate for Susceptibility test
We should avoid placing disks close to the edge of the plate as the zones will
not be fully round and can be difficult to measure. Each disk must be pressed
down with forceps to ensure complete contact with the agar surface or
irregular zone shapes may occur. If the surface of the agar is disrupted in any
way the shape of the zone may be affected.
“Incubation of the plates”
Incubate the Streaked & Antibiotic disk Plates for 18-24 hrs at the 35oC.
Results can be read after 18 hours of incubation.
Note: – Never incubate plates in CO2 as this will decrease the pH of the
agar and result in errors due to incorrect pH of the media.
Note that temperatures above 35°C may not allow the detection of
methicillinresistant Staphylococcus
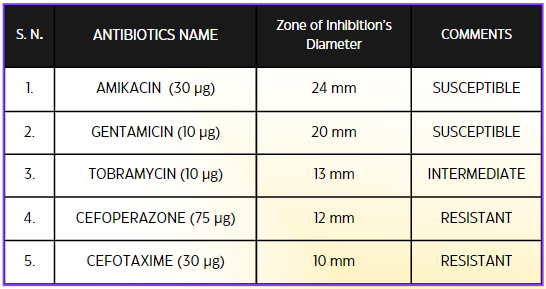
“Measuring zone sizes”
Following incubation, measure the zone sizes to the nearest millimeter using a ruler
or caliper; include the diameter of the disk in the measurement
Measure zone diameters in mm
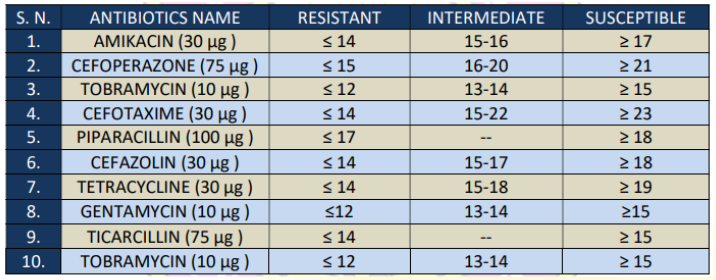
List of Antibiotic Disc used on the MHA Plate for Susceptibility test
“Recommended Antimicrobial Disks and Interpretative Zone Sizes”
Challenges
Antibiotic susceptibility testing (AST) is a critical tool in the field of microbiology and
healthcare, used to determine the effectiveness of antibiotics against bacterial infections.
While it’s a valuable method, there are several challenges associated with it:
Diversity of Bacterial Strains
Emerging Resistance
Slow Results
Complexity of Interpretation
Cost and Resources
Heteroresistance
Lack of Standardization
Address these challenges, ongoing research focuses on developing more rapid and
accurate AST methods, improving standardization, and implementing antimicrobial
stewardship programs to guide appropriate antibiotic use.
Significance
Antibiotic susceptibility testing is a crucial aspect of microbiology and clinical medicine. It
helps determine the susceptibility or resistance of bacteria to specific antibiotics. The
significance of antibiotic susceptibility testing lies in several key areas:
Guiding Treatment Decisions
Preventing Antibiotic Resistance
Tailoring Treatment to the Pathogen
Avoiding Treatment Failures
Monitoring Resistance Trends
Optimizing Antibiotic Use
Preventing Complications
Minimizing Side Effects
In summary, antibiotic susceptibility testing is essential for tailoring antibiotic treatment
to individual patients, preventing antibiotic resistance, and improving overall patient care.
It plays a critical role in both clinical practice and public health efforts to combat the
growing problem of antibiotic resistance..
Challenges
Antibiotic susceptibility testing (AST) is a critical tool in the field of microbiology and healthcare, used to determine the effectiveness of antibiotics against bacterial infections. While it’s a valuable method, there are several challenges associated with it:
Diversity of Bacterial Strains
-
-
-
-
-
-
- Emerging Resistance
- Slow Results
- Complexity of Interpretation
- Cost and Resources
- Heteroresistance
- Lack of Standardization
-
-
-
-
-
Address these challenges, ongoing research focuses on developing more rapid and accurate AST methods, improving standardization, and implementing antimicrobial stewardship programs to guide appropriate antibiotic use.
Also Read
- Bile Salt (Hay’s Sulphur Method)
- Estimation of occult blood in stool by Benzidine method.
-
“Unlocking the Secrets of Urine: A Comprehensive Guide to Urine Examination”
- Glucosuria (Benedict Method)
- Ketone Body (Rotheras, Gerhardt’s and Strip Method)
- Proteinuria (Heat and acetic acid, Sulphur Salicylic Acid, Hellers or Nitric acid, and Esbach albuminometer Method)
- Bence Jones Proteinuria (HCl Method)
- Urobilinogen (Ehrlich Method)
- Bile Pigment (Fouchets Method)
- Occult Blood (Orthotoluidine and Benzidine Method).
- Sedimentation Preparation
- Slide Preparation
- Microscopic Examination.